Navigating Diastolic Dysfunction
A Comprehensive Guide
Diastolic dysfunction, though often overshadowed by its systolic counterpart, plays a pivotal role in heart failure and has become a focus of growing clinical attention. This condition refers to the heart’s impaired ability to relax and fill during diastole, leading to elevated pressures within the left ventricle (LV) and, ultimately, the left atrium (LA). It doesn’t take a reduction in ejection fraction for a heart to fail—diastolic dysfunction can progress silently for years, culminating in diastolic heart failure, a condition marked by breathlessness, fatigue, fluid overload, and fluid buildup in the lungs, abdomen, and legs. This is one of the leading causes of heart failure hospitalizations and an accurate assessment of diastology with echo is key.
Echocardiography is the gold standard for this assessment, offering a real-time evaluation of hemodynamics. While diastolic dysfunction may seem complex, this article will explore the specific echocardiographic measurements needed, following the American Society of Echocardiography recommendations for proper assessment and grading.
We at The Echo Journal use cutting edge technology to deliver echocardiography lessons right to your inbox from across the world. Invest 20 minutes each week to stay updated and access cases and lessons conveniently in our online library.
The Basics
The essential measurements required for the evaluation of diastolic dysfunction include:
Average E/e'
Septal e' velocity and Lateral e' velocity
Tricuspid regurgitation (TR) velocity
Left atrial (LA) volume index
E/A ratio
Peak E velocity
In cases of diastolic dysfunction, the heart has trouble relaxing and filling properly during diastole. Ventricular compliance also plays a role in these cases; when the ventricle stiffens, it cannot stretch to accommodate blood as easily. As a result, higher pressures are needed to fill the heart, leading to elevated filling pressures. This can cause congestion in the lungs or lower extremities and blood backs up due to the heart’s inability to fill. This chronic process of ventricular stiffening is the hallmark of diastolic dysfunction and often associated with hypertension and aging.
Preload and afterload also contribute to diastolic dysfunction. With impaired compliance, the heart struggles to manage increasing preload, and filling pressures increase as a result. Even with normal blood return to the heart (normal preload), a stiff ventricle will have difficulty filling without generating high pressures. On the other hand, increased afterload, such as from high blood pressure, makes it harder for the heart to pump blood out. Over time this added workload can lead to left ventricular hypertrophy, which further stiffens the ventricle and worsens diastolic dysfunction. Together, poor compliance, high preload, and high afterload create a cycle that impairs the heart's ability to relax and fill effectively.
Preload: The initial stretching of the cardiac myocytes from the blood in the heart's ventricles before contraction.
Afterload: The amount of force the heart has to overcome to eject the blood from the ventricles.
ASE Guidelines
Echocardiography is the cornerstone of diastolic dysfunction assessment, allowing non-invasive measurement of filling pressures and ventricular compliance. The ASE guidelines recommend a comprehensive evaluation using multiple parameters.
In patients with a normal left ventricular ejection fraction, if more than 50% of the criteria are positive on the chart above, the second chart is applied. However, in cases of an abnormal LVEF, the first chart is bypassed entirely and we proceed to the chart below.
Mitral Inflow
Mitral inflow assessment is crucial for evaluating diastolic dysfunction, with several key parameters measured using pulsed wave Doppler. To ensure precise measurement, while in the apical 4-chamber view, the Doppler sample volume should be positioned at the tips of the mitral valve leaflets, with careful alignment parallel to the flow. The peak velocities of the E and A waves are key: the E wave reflects early passive filling, while the A wave indicates atrial contraction. According to ASE guidelines, normal E wave peak velocity is typically greater than 0.8 m/s, while the A wave should be less than 0.5 m/s. The E/A ratio, calculated by dividing the peak E wave velocity by the peak A wave velocity, should be greater than 1.0 in normal conditions.
Additionally, the E wave deceleration time (DT), measured from the peak of the E wave to its baseline, provides insights into filling dynamics, with normal values being less than 220 ms. The duration of the A wave is also evaluated to assess the atrial contribution to filling. For this measurement, the Doppler gate may need to be repositioned closer to the mitral annulus. As the heart ages, the LV becomes stiffer and relaxes more slowly resulting in a reduction in the peak E-wave, smaller E/A ratio, and a prolonged E-wave DT.
Tissue Doppler Imaging
Tissue Doppler imaging (TDI) plays a key role in assessing diastolic dysfunction by measuring the mitral annular velocities, particularly the early diastolic velocity (e'). According to ASE guidelines, to properly measure TDI of the mitral annulus, position the Doppler sample volume at the lateral and septal mitral annulus in the apical four-chamber view, ensuring alignment parallel to the myocardial motion for accurate assessment of the e' wave velocities. A reduced e' velocity is a hallmark of impaired myocardial relaxation, a key indicator of diastolic dysfunction. When comparing TDI with mitral inflow measurements, TDI is less influenced by changes in preload, making it a more reliable tool in differentiating between normal and abnormal diastolic function. Combining the E/e' ratio from mitral inflow and annular velocities provides a robust estimate of left ventricular filling pressures, enhancing the diagnostic accuracy for diastolic dysfunction.
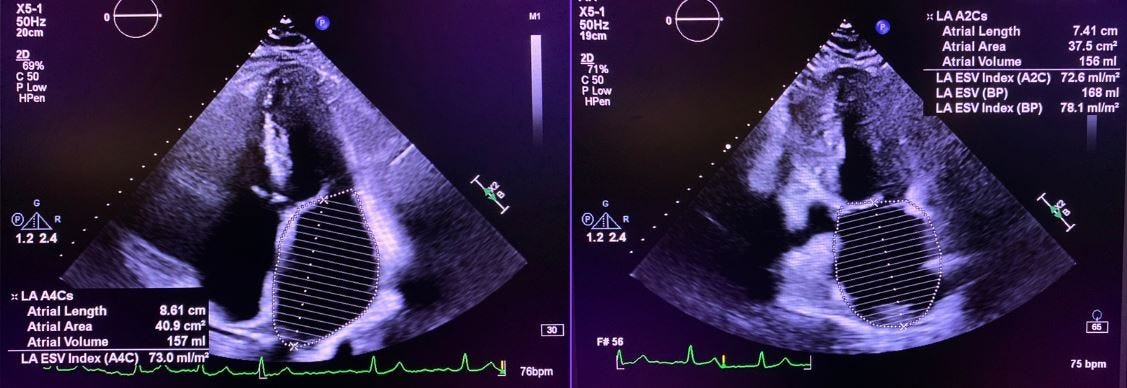
Left Atrial Volume Index
The LA volume index is an important marker in assessing diastolic dysfunction, reflecting the chronic pressure burden on the left atrium due to impaired ventricular relaxation. According to ASE guidelines, an LA volume index greater than 34 mL/m² is considered abnormal and indicative of elevated left ventricular filling pressures. An enlarged LA volume index signifies the long-term effects of diastolic dysfunction and helps in assessing the severity of the condition over time. The LA volume is typically measured using the biplane area-length method. To measure the LA volume index using the biplane method, acquire apical four-chamber and two-chamber views at end-systole, carefully outlining the LA endocardial borders from the annulus to the roof while avoiding the inclusion of surrounding structures, such as the left atrial appendage or pulmonary veins. Ensure that the measurement accurately represents the LA by maintaining a consistent angle and avoiding any interference from adjacent myocardium.
Peak Tricuspid Regurgitation Velocity
Tricuspid regurgitation (TR) is an important consideration in the evaluation of diastolic dysfunction, as it can reflect elevated right atrial pressures that may arise from impaired left ventricular relaxation. The peak velocity of TR, measured using continuous-wave Doppler, is crucial for estimating right ventricular systolic pressure (RVSP), which has potential impacts on the right heart.
According to ASE guidelines, a peak TR velocity greater than 2.8 m/s is typically indicative of significant TR, suggesting that elevated pressures may be present. To ensure accurate measurement, it is essential to align the Doppler beam parallel to the direction of the regurgitant jet, regardless of the view being used, allowing for reliable peak velocity assessment.
Summary
The average E/e' ratio is a key indicator of left ventricular filling pressures, with elevated values suggesting increased pressures that may indicate impaired relaxation.
The assessment of septal and lateral e' velocities aids in determining the extent of diastolic dysfunction, lower velocities indicating diminished ventricular compliance.
The peak TR velocity delivers important information regarding right atrial pressures, with significant elevations suggesting volume overload.
The left atrial volume index serves as a vital marker for chronic diastolic dysfunction, while the E/A ratio, in conjunction with the peak E wave velocity, assists in grading the severity of the dysfunction.
Utilizing these measurements in conjunction with the ASE flow chart facilitates accurate classification of diastolic dysfunction.
Loved this lesson? Take your skills to the next level with The Echo Journal Premium. Gain access to exclusive, in-depth lessons designed to help you master echocardiography and stay at the forefront of your field. With new lessons every week, you’ll be equipped to tackle the toughest cases and refine your technique like a pro.
References
Dewitt, Susan King, et al. Echocardiography: ... From a Sonographer’s Perspective. S.K. DeWitt, 2018.
“Diastolic Dysfunction: Causes, Symptoms and Treatment.” Cleveland Clinic, 4 July 2022, my.clevelandclinic.org/health/diseases/23434-diastolic-dysfunction.
Nagueh, Sherif F., et al. “Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of cardiovascular imaging.” Journal of the American Society of Echocardiography, vol. 29, no. 4, Apr. 2016, pp. 277–314, https://doi.org/10.1016/j.echo.2016.01.011.
Otto, Catherine M. Textbook of Clinical Echocardiography. Elsevier/Saunders, 2019.
Palma, Richard A. Echocardiographer’s Pocket Reference. 2020.







How the diastolic issues affect the individuals with AL Amyloidosis-Cardiac? Can such medical conditions be treated?
helo everyone this very impressive for my basic study for the echocardiogram.. ma still started my career as an echo cardiagrapher this will help me a lot for the further clinical diagnosis ✅